If you’re reading this because you’ve just heard the word Gastroshiza, you’re not alone. Many parents first come across it during a pregnancy scan, and it can feel like the ground shifts under your feet. One minute you’re looking at a baby on an ultrasound, and the next you’re hearing medical terms you’ve never needed before. The good news is that Gastroshiza is a condition doctors understand well, and in most cases, babies can survive and go on to live healthy lives with the right care.
- What Is Gastroshiza?
- Why Gastroshiza Happens (Causes and Risk Factors)
- How Common Is Gastroshiza?
- How Gastroshiza Is Diagnosed
- What Gastroshiza Looks Like at Birth
- Early Signs and Symptoms (Before and After Birth)
- Simple vs Complex Gastroshiza (And Why It Matters)
- The First Hours After Birth: What Doctors Do Immediately
- Gastroshiza Treatment: Surgery and Repair Options
- What Recovery Looks Like After Surgery
- How Long Is the Hospital Stay for Gastroshiza?
- Possible Complications of Gastroshiza
- Survival Rate: What the Data Says
- A Real-Life Style Scenario: What Parents Often Experience
- Long-Term Outcomes: What Life Can Look Like After Gastroshiza
- What Parents Can Expect From Follow-Up Care
- Emotional Survival: The Part People Don’t Always Talk About
- Gastroshiza vs Omphalocele (A Common Confusion)
- Final Thoughts: A Practical Survival Guide for Families
- Conclusion
This guide explains Gastroshiza in a clear, human way. We’ll go through what it is, why it happens, what symptoms and complications can look like, and how treatment works from birth onward. You’ll also learn what survival and recovery typically involve, how long hospital stays can be, and what life often looks like after surgery.
What Is Gastroshiza?
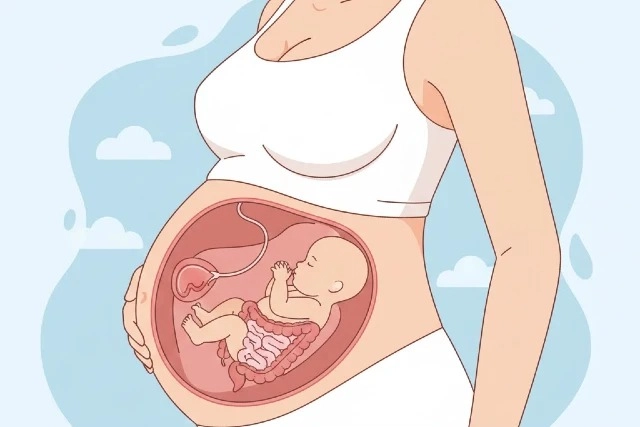
Gastroshiza (more commonly spelled “gastroschisis” in medical literature) is a birth defect where a baby is born with an opening in the abdominal wall, usually just to the right of the belly button. Through that opening, the intestines (and sometimes other organs) develop outside the body with no protective sac covering them. That exposure matters because the bowel is sitting directly in amniotic fluid during pregnancy, which can cause irritation, swelling, and inflammation.
In most cases, Gastroshiza is not linked to an inherited genetic condition. It’s considered a structural birth defect that occurs early in pregnancy when the abdominal wall doesn’t close the way it should.
Why Gastroshiza Happens (Causes and Risk Factors)
Here’s the honest truth: in most pregnancies, doctors can’t point to one single cause of Gastroshiza. Researchers believe it happens due to a combination of factors, including environmental influences and biological changes during early pregnancy.
That said, some risk factors show up consistently across studies.
Young maternal age is one of the strongest known associations. Gastroshiza is more common in younger people who become pregnant.
Tobacco and alcohol use in early pregnancy have also been linked to higher risk in research studies.
Certain infections early in pregnancy, including urinary tract infections and some sexually transmitted infections, are also associated with increased risk.
It’s important to say this clearly: many babies with Gastroshiza are born to parents with no known risk factors at all. So while risk factors help researchers understand patterns, they don’t always explain individual cases.
How Common Is Gastroshiza?
Gastroshiza is considered rare, but it’s not extremely rare. A major estimate often cited in U.S. healthcare sources is that it affects about 1 in 2,000 babies.
It has also been reported that prevalence has increased over time in multiple parts of the world, which is why it continues to be actively studied.
How Gastroshiza Is Diagnosed
Most of the time, Gastroshiza is diagnosed during pregnancy.
A prenatal ultrasound often shows bowel loops outside the baby’s abdomen. Doctors may also notice increased amniotic fluid levels or changes in bowel appearance.
Some blood screening tests can show abnormal results, including elevated maternal serum alpha-fetoprotein (AFP), which can be associated with open abdominal wall defects.
If a baby is not diagnosed before birth, Gastroshiza becomes obvious immediately after delivery, because the intestines can be seen outside the body.
What Gastroshiza Looks Like at Birth
Babies with Gastroshiza are usually born with intestines outside the abdomen through a small opening near the belly button. The exposed bowel can appear swollen, thick, and irritated. In more severe cases, other organs such as the stomach can also protrude.
This can look frightening if you’ve never seen it, but neonatal teams are trained to handle it quickly. The first minutes after birth focus on keeping the bowel protected, keeping the baby warm, and stabilizing breathing and circulation.
Early Signs and Symptoms (Before and After Birth)
During pregnancy, there are usually no symptoms a parent “feels.” The signs are typically seen on imaging.
After birth, symptoms are related to how the intestines are functioning and how quickly the baby can be stabilized and repaired.
Babies with Gastroshiza may have trouble feeding at first. They may not tolerate milk immediately because the bowel needs time to recover after surgery and because exposed intestines can be slow to function.
Some babies may have breathing difficulty early on, especially if the abdomen becomes tight after closure and pushes on the diaphragm. That’s one reason surgeons carefully choose between immediate closure and staged closure.
Simple vs Complex Gastroshiza (And Why It Matters)
Doctors often describe Gastroshiza as either “simple” or “complex.”
Simple cases involve exposed bowel that is still healthy and functioning, without major damage or blockages.
Complex cases involve intestinal complications such as atresia (a blockage or missing segment), perforation, necrosis, or severe inflammation. Complex cases usually require longer hospital stays, more surgeries, and longer nutrition support.
This distinction matters because it affects the recovery timeline and long-term outcomes.
The First Hours After Birth: What Doctors Do Immediately
Right after delivery, the medical team focuses on stabilization.
The bowel is covered with sterile protective material to prevent heat loss and moisture loss. Babies with exposed intestines lose fluids quickly, so IV fluids are started early.
The baby is kept warm and monitored closely. A tube is often placed through the nose into the stomach to remove air and fluid, reducing pressure in the intestines and helping prevent vomiting or aspiration.
Once the baby is stable, a pediatric surgeon evaluates the bowel and decides on the best surgical approach.
Gastroshiza Treatment: Surgery and Repair Options
Treatment for Gastroshiza is surgical. The goal is to place the intestines back inside the abdomen and close the opening, but the approach depends on the baby’s condition and how swollen the bowel is.
Primary Closure
In primary closure, the surgeon returns the intestines into the abdomen and closes the opening in one procedure. This is usually possible when the bowel is not too swollen and the abdominal cavity can handle the pressure without compromising breathing or blood flow.
Staged Closure Using a Silo
If the bowel is too swollen or if immediate closure would be too tight, doctors use a silo. A silo is a sterile pouch placed over the exposed intestines. Over several days, the bowel is gradually guided back into the abdomen as swelling decreases. Then the opening is closed.
This staged approach is common and often done right at the bedside in the NICU, depending on the hospital’s protocol.
What Recovery Looks Like After Surgery
This is the part many families don’t realize until they’re living it: after repair, the biggest challenge is often not the surgery itself. It’s getting the intestines to “wake up” and work normally.
In the early days, babies are usually fed through IV nutrition, called parenteral nutrition, because the intestines may not be ready to digest milk.
Feeding is introduced slowly. Some babies tolerate breast milk or formula quickly, while others need more time, especially if the bowel was inflamed or if complications exist.
Recovery involves monitoring for infection, checking bowel function, watching weight gain, and managing fluid and electrolyte balance. Most babies remain in the NICU for weeks, and some for longer depending on complexity.
How Long Is the Hospital Stay for Gastroshiza?
Hospital stays vary widely. Many babies with simple Gastroshiza spend several weeks in the hospital, primarily to support feeding and bowel recovery.
Complex cases may require longer stays, especially if multiple surgeries are needed or if the baby develops complications such as infections or short bowel syndrome.
Parents often hear doctors talk about “discharge goals,” which usually include stable breathing, full feeding by mouth or tube, weight gain, and absence of serious infection.
Possible Complications of Gastroshiza
Most babies survive, but Gastroshiza can come with complications. Knowing them doesn’t mean expecting the worst—it just helps you understand what doctors monitor so closely.
Infection and Sepsis
Because the intestines are exposed, infection risk is higher, especially before and during repair. Sepsis is one of the most serious concerns, which is why babies are monitored closely and often receive antibiotics.
Bowel Function Delays
Many babies take time before their intestines begin working normally. This delay can result in prolonged dependence on IV nutrition.
Necrotizing Enterocolitis (NEC)
Babies with bowel injury or reduced blood flow are at risk for NEC, a serious intestinal condition that affects premature and medically fragile infants.
Intestinal Atresia or Blockage
Some babies are born with blockages or narrowed segments of intestine. These cases are considered complex and may require additional surgery.
Short Bowel Syndrome
In severe cases where sections of intestine are damaged and must be removed, babies may develop short bowel syndrome, which can cause long-term digestion and nutrition challenges.
Survival Rate: What the Data Says
This is one of the first questions families ask, and it’s completely understandable.
In well-resourced healthcare settings, survival for treated Gastroshiza is now typically over 90%, and some modern reports note survival above 95%.
This improvement is considered one of the major success stories in pediatric surgery, largely due to advances in neonatal intensive care, use of silos, parenteral nutrition, improved ventilation, and better infection control.
However, outcomes are not equal everywhere. Studies show survival remains significantly lower in low- and middle-income countries due to limited access to neonatal intensive care and surgical resources.
A Real-Life Style Scenario: What Parents Often Experience
Many parents describe the same emotional rhythm.
First comes diagnosis, often during the 18–20 week anatomy scan. Shock is common, along with the fear of the unknown. Then comes planning, because most families are referred to a high-level hospital with pediatric surgery and NICU care.
After birth, parents usually can’t hold the baby immediately, because stabilization happens quickly. Sometimes they can touch the baby’s hand while doctors cover the bowel and secure medical support.
The NICU journey becomes a pattern of small wins. The first stable breathing day. The first successful feeding. The first time the baby gains weight consistently. Those moments matter because they are signs the body is recovering.
Long-Term Outcomes: What Life Can Look Like After Gastroshiza
The long-term outlook depends on whether the case was simple or complex.
Many children with simple Gastroshiza recover well and live normal lives. They may have a belly scar, and they may have mild digestive sensitivity early on, but many catch up developmentally over time.
Some children may experience feeding difficulties in infancy, slower growth in the first year, or occasional bowel issues such as constipation or reflux.
Complex Gastroshiza cases may require longer follow-up, especially for growth monitoring, nutrition support, or bowel function. Some may require additional surgeries for adhesions or blockages.
Research reviews show that as survival improves, healthcare teams focus more on long-term quality of life, nutrition, growth, and developmental monitoring.
What Parents Can Expect From Follow-Up Care
Follow-up usually includes pediatric surgery visits, nutrition monitoring, and sometimes gastroenterology care if feeding or absorption remains difficult.
Doctors may monitor growth carefully, because babies recovering from bowel surgery often need extra calories to catch up.
Some children may need temporary tube feeding. Others transition fully to oral feeding with time.
The best indicator doctors look for is steady progress: growing, feeding, and meeting developmental milestones. Most families find that once feeding becomes stable, life becomes much easier.
Emotional Survival: The Part People Don’t Always Talk About
A lot of parents focus on the baby’s survival, but emotional survival matters too.
Living through a NICU journey can be exhausting. The stress of alarms, medical terms, surgery discussions, and uncertainty can weigh heavily.
Many families find strength in routines, learning the basics of NICU care, and celebrating small improvements rather than waiting only for discharge day.
The hardest part is often the waiting. But waiting is also where healing happens.
Gastroshiza vs Omphalocele (A Common Confusion)
Gastroshiza is often confused with another abdominal wall defect called omphalocele, but they are different.
In omphalocele, the organs protrude through the belly button area but are covered by a thin sac. Gastroshiza usually has no covering sac, and the opening is typically beside the belly button.
Doctors treat both conditions differently, which is why correct diagnosis is important.
Final Thoughts: A Practical Survival Guide for Families
If you’ve been told your baby has Gastroshiza, the first thing to remember is this: you’re facing something serious, but you’re not facing something hopeless.
Modern medicine has made Gastroshiza highly treatable in many healthcare systems, with survival rates above 90% and often above 95% in well-equipped hospitals.
The road involves surgery and patience. It often involves weeks in a NICU. It can involve feeding challenges. But for many families, it also ends with a baby who grows, heals, and eventually lives a life that looks normal again.
Understanding this condition is also closely connected to how gastroschisis is classified and treated across modern pediatric surgery systems, and why early diagnosis improves planning and outcomes.
Conclusion
Gastroshiza can feel overwhelming at first, especially when it is discovered during pregnancy or immediately after birth. But with modern neonatal care, advanced surgical options, and careful monitoring in the NICU, most babies with Gastroshiza have a strong chance of survival and long-term recovery. The journey often involves surgery, patience, and gradual feeding progress, yet many children go on to live healthy, active lives once their intestines heal and their growth stabilizes. Understanding Gastroshiza, its causes, symptoms, treatment steps, and recovery timeline helps families feel more prepared and confident throughout the process, turning fear into clarity and uncertainty into hope.